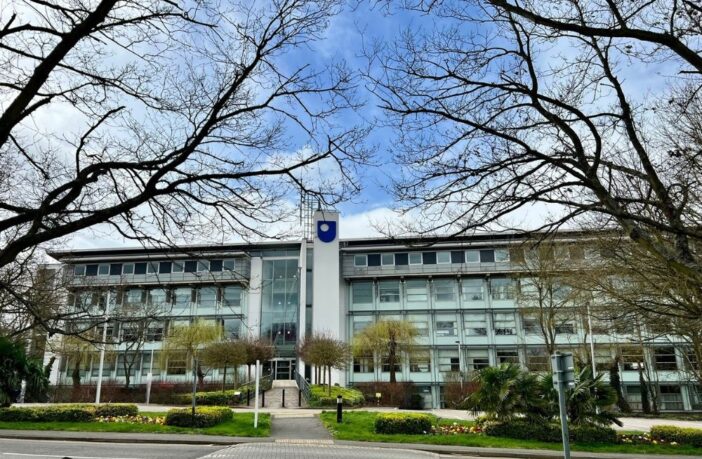
A new study published today and led by The Open University (OU) has identified significant areas for improvement in the care for transgender adults within the NHS.
The report, titled ‘Improving the integration of care for trans adults: ICTA a mixed-methods study’, has been published in the journal Health and Social Care Delivery Research by a team of researchers from the Open University’s Business School, School of Health, Wellbeing and Social Care, and School of Psychology and Counselling.
The team worked alongside independent researchers and experts from Yorkshire MESMAC, the LGBT Foundation and other third sector organisations. The research has been funded by the National Institute for Health and Care Research (NIHR).
The study explored the current landscape of trans healthcare in the UK and identified key factors contributing to both positive and negative experiences. Researchers interviewed 110 trans people who had received NHS care, with a further 23 people attending focus groups. 55 interviews investigated the views of National Health Service and voluntary-sector staff involved in delivering trans health care.
The new report highlights several factors that can lead to fragmented or poor care for trans people:
- Disrespectful treatment in general practice: Transgender individuals have reported that they face discrimination and a lack of understanding from their GP practices.
- Inadequate funding: Limited resources restrict the availability and quality of services.
- Lack of support during waiting times: The lengthy wait times for Gender Identity Clinic (GIC) appointments can leave individuals feeling unsupported and isolated.
- Challenges with GIC assessments: The current diagnostic process can be lengthy, complex, and stressful.
- Disjointed collaboration: Communication and collaboration between GICs and GP practices regarding hormone therapy can be inconsistent.
- Limited access to NHS psychological support: Trans people often struggle to access appropriate mental health services.
The report proposes several key recommendations to improve the integration and quality of trans healthcare within the NHS:
- Training in trans healthcare for GPs: Equipping GPs with the knowledge and skills to provide respectful and informed care.
- Peer support workers: Integrating third-sector peer support into NHS services can offer valuable emotional and practical assistance to trans individuals.
- Collaborative GIC assessments: Shifting towards a more collaborative approach to assess individual needs and treatment options.
- Regional GP-led hormone therapy clinics: Bringing hormone therapy provision closer to communities and integrating it into mainstream healthcare.
- Focus on support, not assessment: Replacing the emphasis on assessment in psychological services with a focus on providing supportive and affirming care.
The research team stress the importance of understanding the diverse needs and experiences of trans adults to ensure effective and accessible healthcare.
Professor Richard Holti, project leader from The OU Business School, said:
“We have explored how to improve care both immediately and in the longer term, and two things stand out. First, existing initiatives to integrate support for trans people into primary care and GP services can be strengthened. Secondly, the NHS can build on recent developments in assessing trans people for treatment, making the experience more collaborative and in many cases simpler. The goal is to combine better care with better use of NHS resources.”
Jay Stewart, Chief Executive Officer of Gendered Intelligence, added:
“Trans, non-binary and gender questioning people are entitled to timely, age appropriate, high-quality healthcare under the NHS. This important research underscores the negative experiences of trans people, whether treading water on seemingly endless waiting lists or being treated without dignity and respect in the doctor’s office. These findings make it clear: We need urgent change for trans healthcare now.”
Dr Paul Martin OBE, Chief Executive of LGBT Foundation, said:
“This report provides a rigorously evidenced picture of what can go wrong in how the NHS provides care for trans adults, as well as indicating what good care looks like. The report analyses recent initiatives to improve services for medical transition and points above all to the need to integrate transition-related care much more closely with general healthcare. The recommendations around the need for culturally competent education within primary care are especially worthy of note. It should provide a valuable input to the forthcoming review of adult gender services in England.”
The ICTA research team will soon be launching online courses based on their findings, aimed at both healthcare staff and individuals seeking or supporting trans healthcare. These resources aim to contribute to improved awareness, understanding, and service delivery for trans adults within the NHS.