The People vs the NHS: Who Gets the Drugs? on BBC2 at 9pm on Wednesday 27 June, is an Open University and BBC co-production, following the incredible story of the battle for HIV drug pre-exposure prophylaxis, or PrEP, on the NHS.
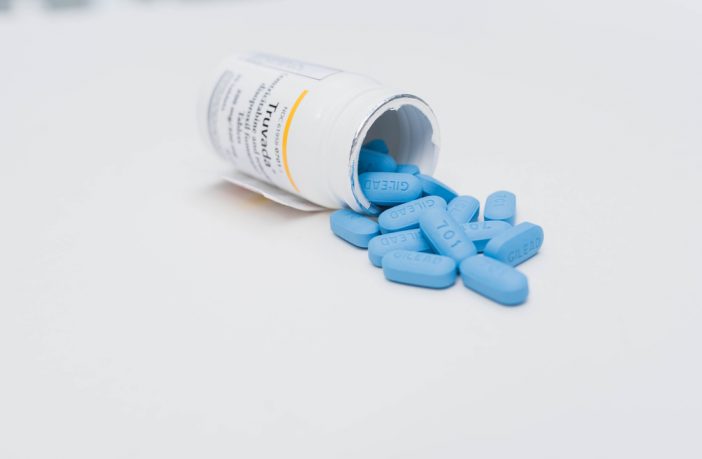
People at very high risk for HIV take PreP daily to lower their chances of getting infected by the virus. When taken consistently, it can stop HIV from taking hold and spreading throughout the body, and experts believe it could end the HIV and AIDS epidemic. But in 2016 the NHS, after 18 months of consultation, made the controversial decision that they could not fund it.
The programme tells the story of the legal fight which followed and saw doctors, activists and AIDS charities come together to overturn the NHS decision. The NHS is now conducting a clinical trial to test it. The programme explores the hugely complex decisions facing the health service in one of the most difficult periods in its history.
As you might expect, it’s not as simple as taking a daily pill – there are so many factors involved in the story, and one factor is social inequality. Here, OU Senior Lecturer in Public Health Dr Peter Keogh explores whether PrEP really is the scientific breakthrough to end the HIV epidemic in a world filled with social inequalities…
It’s not as simple as a pill a day

The news that a daily pill can protect us from becoming infected with HIV is momentous and many people have started to talk about PrEP as a ‘silver bullet’: the scientific breakthrough with the potential to end the HIV epidemic. But can any medical breakthrough, any pill, ever be enough to end an epidemic that has raged for over thirty years, claiming the lives of 35 million people around the world?
The story of the struggle for PrEP in England shows that pills alone are not sufficient. The government needs to be persuaded that funding PrEP is worthwhile and we need to fight to make it available to those who need it. People also need to be educated about PrEP, they need to have confidence that it will work and they need to know how to use PrEP so that it is most effective.
But there are more entrenched battles to fight.
Inequality and impact
Like many global epidemics, HIV does not affect all people equally. HIV has a disproportionate impact on poorer and less educated people and those from marginalised and stigmatised groups. Across the world, HIV lays the heaviest burdens on women, sex workers, gay and bisexual men and migrants.
We see this pattern in the UK where the two groups that make up the clear majority of HIV infections are gay and bisexual men and Black African migrants. Gay communities have long been the target of virulent homophobia, only recently gaining human rights that the rest of us take for granted: the right to marry and form a family and the right to protection from discrimination. Likewise, African migrant communities have borne the brunt of racism and xenophobia which has worsened in recent years with the UK’s ‘hostile environment policy’. Many have found themselves stripped of their rights when they arrived in the UK.
The evidence from Public Health has long shown that when people are subject to stigma and discrimination, when they are poor, when their rights are denied and when they feel powerless, they are less able to protect themselves and their loved ones from disease and ill health. To be healthy, people need a basic income, education, independence, self-determination and their fundamental human rights guaranteed.
“So, although drugs can help to control the HIV epidemic, they can’t really deal with the factors that fuel the epidemic in the first place.”
We have a pill that can stop us getting infected, a pill that can stop us getting ill and perhaps one day, we’ll have a pill that can cure HIV. But there will never be a pill that cures poverty, inequality, stigma, discrimination and human rights abuses and because of this, no pill will ever be enough to end the HIV epidemic.
Part of a bigger picture
So, what is needed, and what is the role of treatments like PrEP? Global health agencies like the World Health Organisation and UNAIDS have long recognised that dealing with stigma, poverty and inequality are as important as medical treatments in tackling the HIV epidemic. In other words, PrEP will have little chance of reaching its potential if people don’t know about it, can’t afford it, are more concerned with feeding themselves and their families than they are about contracting HIV, feel powerless or simply feel that their lives aren’t worth it. But likewise, tackling stigma, discrimination and poverty on their own is not enough to end the HIV epidemic. We desperately need the pills too.
There is so much to celebrate in the world of HIV. Those of us living with HIV and successfully on treatments can expect a normal healthy life expectancy – and we can’t pass HIV on to our sexual partners. Those of us at risk for HIV through the sex we have and the people we love can protect ourselves with condoms and PrEP. But we need to remember that this is just part of a bigger picture that we must keep this in our sights if we are ever to end the HIV epidemic.
This article was first published on OpenLearn.
Find out more
Test your knowledge about HIV and AIDS by completing our interactive quiz
Learn more about public health and infectious disease using our free online course
Read more about Peter’s research group, the Reproduction, Sexualities & Sexual Health Research Group (RSSH)